EMULSIFIERS could cause inflammatory bowel disease and metabolic syndrome by altering the gut microbiota composition and localisation and inducing intestinal inflammation, according to a new research published in Nature.
Findings by a team from the Georgia State University Institute for Biomedical Sciences suggest emulsifiers disturb the gut microbiota, the diverse population of 100 trillion bacteria inhabiting the intestinal tract, which then causes inflammatory bowel disease (IBD) and metabolic syndrome. Research on mice results show that changes in the species composition of the gut microbiota resulted in abnormal immune systems, which then triggered chronic colitis. Emulsifiers induced low-grade or mild intestinal inflammation and metabolic syndrome, characterised by increased levels of food consumption, obesity, hyperglycemia, and insulin resistance, in mice with normal immune systems. Germ-free mice, which lack a microbioata, did not exhibit any effects of emulsifier consumption.
Transplanting microbiota from emulsifiers-treated mice to germ-free mice resulted in the transfer of some parameters of low-grade inflammation and metabolic syndrome, indicating a central role for the microbiota in mediating the adverse effect of emulsifiers.
The research team, which was led by Drs Benoit Chassaing and Andrew T. Gewirtz, tried to model the consumption of numerous emulsifiers used in almost all processed foods by feeding mice with two very commonly used emulsifiers, polysorbate 80 and carboxymethylcellulsose. The results show the species composition of the gut microbiota was changed, became more pro-inflammatory and had increased capacity to digest and infiltrate the dense mucus layer lining the intestine, which is normally largely devoid of bacteria. Further, the changes in bacterial species allowed bacteria to express more flagellin and lipopolysaccharide, which can activate the immune system’s pro-inflammatory gene expression.
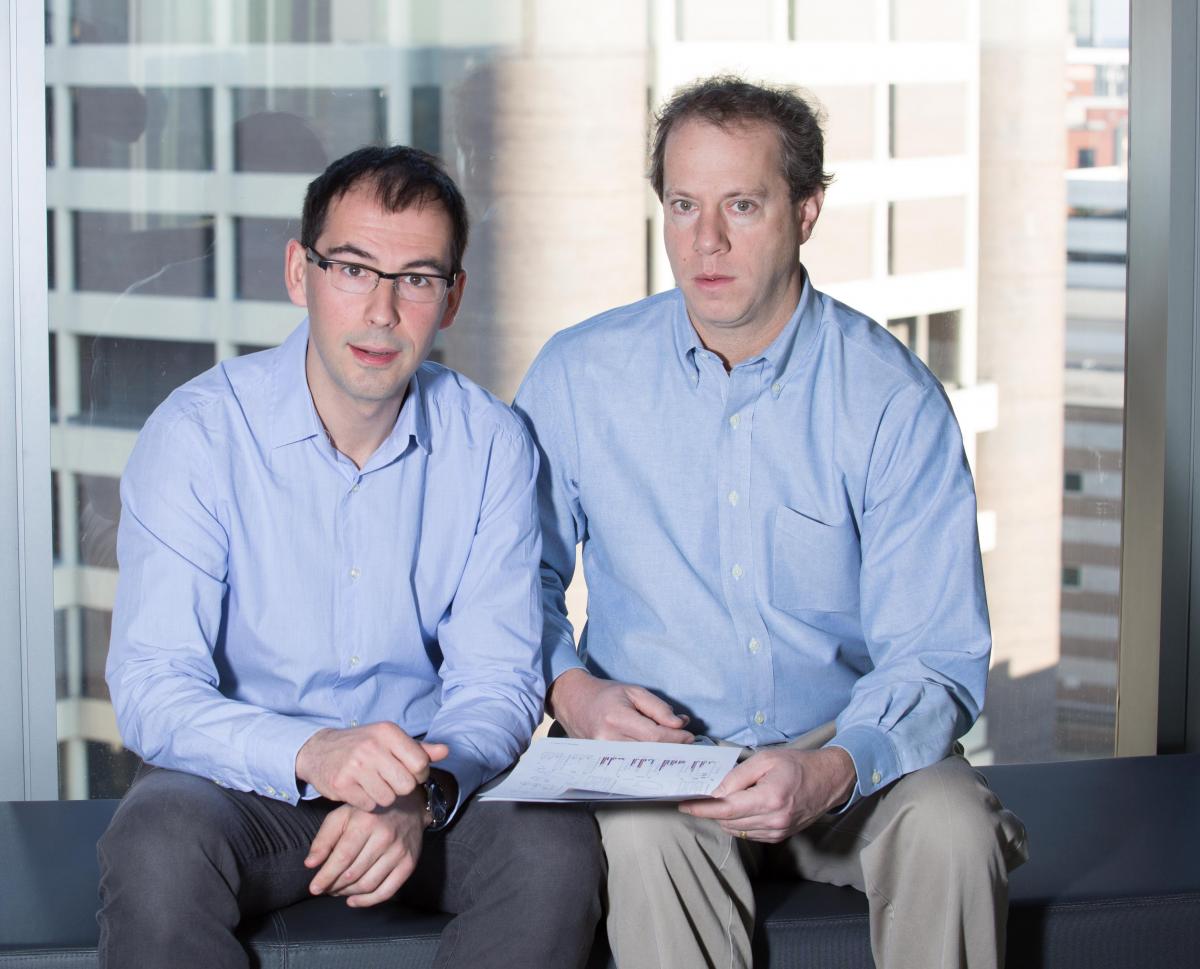
From left, Dr Benoit Chassaing and Dr Andrew T. Gewirtz
The team is testing additional emulsifiers and designing experiments to look into how emulsifiers affect humans. Similar findings would indicate the link between the food additive and obesity and its interrelated consequences and a range of diseases associated with chronic gut inflammation.
Cases of IBD and metabolic syndrome have been rising since the mid-20th century. IBD, which includes Crohn’s disease and ulcerative colitis, afflicts millions of people and is often severe and debilitating. Metabolic syndrome is a group of very common obesity-related disorders that can lead to type-2 diabetes, cardiovascular, and/or liver diseases.
According to Dr Gewirtz, a key feature of IBD and metabolic syndrome is the alteration of the gut microbiota in a manner that promotes inflammation. Hypothesising that emulsifiers, which are added to most processed foods to aid texture and extend shelf life, might affect the gut microbiota to promote these inflammatory diseases, Drs. Chassaing and Gewirtz designed experiments in mice to test this possibility.
“The dramatic increase in these diseases has occurred despite consistent human genetics, suggesting a pivotal role for an environmental factor. Food interacts intimately with the microbiota so we considered what modern additions to the food supply might possibly make gut bacteria more pro-inflammatory,” Dr. Chassaing said.
The findings suggest current means of testing and approving food additives may not be adequate to prevent use of chemicals that promote diseases driven by low-grade inflammation and/or which will cause disease primarily in susceptible hosts.
Detailed mechanisms underlying the effect of emulsifiers on metabolism remain under study. Nevertheless, the research noted the importance of avoiding excess food consumption.
“We do not disagree with the commonly held assumption that over-eating is a central cause of obesity and metabolic syndrome. Rather, our findings reinforce the concept suggested by earlier work that low-grade inflammation resulting from an altered microbiota can be an underlying cause of excess eating,” Dr. Gewirtz stated.
This study included contributions from Emory University, Cornell University, and Bar-Ilan University in Israel. It was funded by the National Institutes of Health and Crohn’s & Colitis Foundation of America.
Photo © Johanna Goodyear | Dreamstime Stock Photos
Munkaw Chaos Girl
 iConnectHub
iConnectHub
 Login/Register
Login/Register Supplier Login
Supplier Login